The year I went to war with my body
Between the ages of twenty and forty-five, I went to the doctor maybe ten times. I had a few uneventful physicals. I needed six stitches after catching an elbow once playing basketball. And I had an infection in my leg that went away after a few days on an antibiotic. That was it. I lived a very healthy twenty-five years. I joked about how much money insurance companies were surely making off of me.
That changed abruptly in the summer of 2022, during my 46th year, when I was diagnosed with testicular cancer.
August, 2022
(Disclaimer - this essay makes frequent references to the male anatomy. Specifically, my male anatomy.)
Washing my nether regions in the shower, I noticed a small lump on the outside of my right testicle. My wife, a family practice doctor who usually (and rightfully) dismisses my medical inquiries with a “you’re fine,” was immediately concerned.
So I scheduled an urgent care visit for the following week. The urgent care doctor sent me to get a scrotal ultrasound the next day (which was a not-so-pleasant and surprisingly long 30 minutes…). The day after that, I saw a urologist who was fairly certain within minutes that I had a cancerous tumor on my right testicle. This was confirmed by a blood test which showed elevation of three hormone markers associated with testicular cancer.
Cancer. Less than a week from “huh, what’s that?” to being diagnosed with cancer.
The next week, I had a CT scan of my abdomen which, to our relief, indicated that there was not yet any sign of spread to the rest of my body. But we needed to move quickly. I needed immediate surgery to remove my right testicle (hereafter known as “The Traitor”) and the tumor growing on it, in the hopes of preventing it from spreading to the rest of my body.
September, 2022: Surgery #1
I was set to go under the knife at Beth Israel hospital in Boston on Sept 7, 2022 - just ten days after my first appointment. Beth Israel worked to schedule the operation quickly to try and minimize any further opportunity for the cancer to spread. The surgery, called a Radical Orchiectomy, would entail knocking me out for a few hours and then making a ~4-inch incision along my waistline through which The Traitor and its spermatic cord would be removed.
This was my first time ever having major surgery. I had an anesthesiology IV inserted into my arm, was wheeled on a gurney into the Operating Room, made nervous small talk with the nurses and doctors…and woke up a few hours later in a complete anesthesia-induced fog. Waking up from general anesthesia is a trip - it’s like coming out of a deep sleep, but even though you are trying to wake up, you just can’t for about an hour…it’s very strange.
After I regained my senses, less than 5 hours after I arrived, I was free to leave (well, most of me anyway…good riddance, Traitor!). I slept at home that evening.
I could walk (or, more accurately, shuffle) but was in a lot of pain for about a week and couldn’t do much besides lie on the couch. But within a week, I was able to walk around the block and resume my Uber-Dad responsibilities of driving my two daughters around greater Boston to soccer and school events.
A few days after the surgery, the pathology report came back from the analysis (i.e. dissection) of The Traitor and indicated that I was “Stage 1B” - which meant there was no sign of spread, but I had an aggressive blend of cancers (specifically: Non-Seminoma Yolk Sac and Embryonal Carcinoma) and some indication that the cancer was starting to move up the spermatic cord towards the rest of my body. All of this meant that I had an elevated risk of recurrence. The (soon to be moot…) options presented were:
- One “adjuvant” cycle of chemotherapy (3 weeks) to beat back any lingering cancer cells, with BEP (Bleomycin, Etoposide, Cisplatin) - this would mean less than a 5% chance of recurrence.
- Another major surgery (RPLND - Retroperitoneal lymph node dissection) to remove lymph nodes from my abdomen that may have cancer that wasn’t picked up in the CT scan - most likely also be a low single digit probability of recurrence.
- No further treatment. Just periodic surveillance but with a high probability (~50%) of recurrence, which would then require more intense treatment (at least 9 weeks of chemo and possibly additional surgery as well).
We decided to go for the Adjuvant Chemo and planned for it to start in early November. I talked with doctors at Beth Israel and Dana Farber, and both agreed this seemed like a prudent approach.
October, 2022: Recovery #1
I was able to start being active again and jogging, playing basketball and tennis, though I was really out of shape from a month of doing pretty much nothing. I enjoyed the strangely warm New England fall. After I sold FutureMe, I had decided to “pre-tire” for a while, so I didn’t have any need to balance a “real job” through this ordeal, for which I felt extremely fortunate.
Testicular cancer afflicts just approximately ten thousand men in the US every year. The average age of a TC patient is 33, and as such, I was on the (way) older side of the distribution curve. In fact, when I first told my wife that I was concerned about a lump, she said “you’re too old for testicular cancer.” But once we’d confirmed that I did have TC, she also said “if you’re going to get cancer, that’s the one to get,” as the 5 year survival rates are the highest amongst all types of cancer at about 95%. That being said, cancer is a scary word. And even a 5% mortality rate is significant - roughly double the 2.7% mortality rate of American military personnel who served in Vietnam. A 1/20 chance of not surviving for more than 5 years was unnerving, to say the least.
I told many of my friends about what I was going through, and I learned about six different testicular cancer cases amongst an extended friend-of-friends network. I was able to connect with a few of them to hear their stories and learn more about what I was up against and could expect over the next few months.
November, 2022
Chemo. Or not…
I was slated to start my week of chemo on Monday, November 14. The week prior, I did a series of tests to prepare and ensure my readiness for chemo. Chemotherapy involves effectively putting poison into the body that will indiscriminately attack fast-growing cells, hopefully including cancer, but also including hair and other “collateral damage” cells. As such, the “cure” includes associated risks in and of itself. The readiness tests included a breathing strength test (as a baseline, as the “B” carries some risk of having adverse side effects on lungs), as well as another CT scan (the 2nd time) to look for any new unusual growths in the abdomen, as well as a blood draw (3rd time) to look for elevated levels of hormones that could indicate the cancer had spread.
Here is a fun anecdote, just tangentially related to my cancer care. I also had to get a COVID PCR test, and when I showed up at BI’s outdoor testing site on Sunday morning, the staff started enthusiastically cheering for me as I rode up on my bike. I was humbled but confused. It turned out I was literally the very last person to ever get a COVID test at this outdoor site, out of presumably many thousands of people over several years, because it was the site’s last day of operation. The exuberant staff took selfies with me and even gave me a wrapped present, which is a very nice Beth Israel coffee mug that I use regularly for my morning coffee!
I was scared of chemo. But my spirits were lifted when some of my tennis friends sent me a video they had made from Chris Mullin (former NBA star for the Warriors - my team growing up!) wishing me luck. I also had a bunch of my basketball-playing buddies sign up to bring over food during my treatment.
I arrived on Monday and nervously checked in for a full week of five full days of chemo (5 days x 6 hours each) with an iPad loaded up with 4 seasons of Yellowstone (which is actually not that good after the first season).
I met the nurse who would be administering the chemo. She inserted an IV into my arm, and I was literally minutes away from starting the drip of the chemotherapy drugs into my body…when my oncologist arrived and said that the CT scan from Friday showed signs of enlarged lymph nodes in my abdomen. The cancer had indeed started to spread, and I was now in Stage 2 rather than Stage 1.
So we needed to reevaluate our treatment options. I would need to do either 3 cycles of chemo (vs. the 1 we almost started) of BEP Chemo or the same RPLND Lymph Node surgery that I had originally considered, the findings of which would determine what, if any, additional chemo would be prudent.
Given the new information and the uncertainty, we decided to quite literally “pull the plug” (or the “IV,” as it were) and reconsider our options. As she removed the IV from my arm, my nurse said that in ten years on the job, this was the first time that she’d ever had this last-minute aversion happen and said jokingly, “I hope I never see you again!” (which unfortunately was not true…). Shell-shocked, I left the treatment center and walked home three miles along the Emerald Necklace during the uncharacteristically warm November day.

Surgery #2
After consulting with Anna and my doctors, this time we decided to go with the Lymph Node surgery, knowing the outcome from that would likely be 2 cycles (6 weeks) of Chemo, but with an outside chance I wouldn’t need any chemo at all. The surgery would also let us know more about the enlarged lymph node, as there was a chance that it was a cancer type (Teratoma) that does not respond well to chemo. The doctors worked hard to get this second surgery scheduled for November 30, because as is always the case with cancer treatment, time is of the essence.
I showed up at 8:30 am on Nov. 30 for the second major surgery in 3 months. The specific procedure consists of laparoscopic (robotically assisted!) surgery through 6 small incisions in a half circle around the right side of my belly button. In most cases, this same surgery entails a giant 25-inch incision from the waist, around the belly button, and all the way up by stomach and sternum. As I did many times during this journey, despite it being a sucky experience, I reflected and felt grateful for the recent medical developments that enabled modern and effective treatment.
I was under general anesthesia for almost 10 hours, which was about twice as long as was scheduled. Apparently, Anna was (justifiably) quite on edge for those last few hours, as she was supposed to get the “all clear” call at 2 and didn’t until 5:45. 41 lymph nodes had been removed. And at one point, my aorta had been nicked, and apparently, it was touch and go about whether an emergency blood transfusion would be necessary.
Just like in September, I woke in a complete daze, and it took 2 hours to fully regain awareness and consciousness. My shoulders hurt like crazy from all of the air they had blown into me to inflate my belly and give the surgeon more room to operate. I had to stay the night in the hospital for monitoring and was discharged the following afternoon.
The first 5 days at home were downright brutal. I couldn’t sleep well and was in a lot of pain. It felt about how you’d think it would feel if your insides had been poked and prodded and sliced for ten hours. I had six bandages around my belly button leaking blood and pus. I was pretty useless.
By about Day 7, I could feel myself starting to get better, but I felt a bit of “déjà vu” from September, as once again I had to work my way back to normalcy over the course of a month or so.
December, 2022
Recovery #2
The pathology report came back on December 2. Of the 41 lymph nodes removed during surgery, 6 had cancer. The tumors were all relatively small. One of the tumors (the largest one) was of the Teratoma variety, which is resistant to chemo. So it was actually pretty great that we opted for surgery rather than just chemo alone.
But because there were 6 cancerous tumors found, I needed to do additional chemotherapy treatment, as having more than 5 tumors in the lymph nodes was the cut-off in the treatment rubric. So I was scheduled to start 2 cycles (6 weeks) of chemo starting on January 9.
As an aside, the crazy thing with this entire experience is that I never had any symptoms of anything directly related to the cancer, other than the mildly curious/annoying lump that I discovered back in August. I was doing all the active things I liked to do right up until the first surgery (I literally played tennis that morning), and I was back in action a month after the first surgery and doing what I like to do in October and November. It was tempting at times to just ignore the whole thing and pretend I was fine. But exponential growth is scary, and intellectually, I knew we needed to act aggressively to treat it. But emotionally, I had many moments when I just wanted to forget it and live my normal life.
For Christmas, my wife bought me “The Emperor of all Maladies: A Biography of Cancer,” which is an exhaustively researched account of how the treatment of cancer has iteratively evolved beyond crude and even barbaric surgery to include precision surgeries, targeted radiation, specific chemotherapy regimens, and mitigations to the side effects of all of these treatments.
As I read these detailed accounts of the many dozens of doctors, researchers, and policy advocates, hardly any of whom I’d heard of before, iteratively advancing the state of cancer care, I felt profound gratitude for their grit chipping away against this insidious disease. One of the stories in the book is that of a Dr. Einhorn, who at Indiana University in the early 1970s, discovered the chemotherapy treatment regimen that reliably cures early-stage testicular cancer. If I had lived even just 50 years ago, my Stage 2 diagnosis would have meant something like a 20% survival rate. But today, even in Stage 2, it is 95%.
January, 2023
Chemotherapy. For real this time…
I was set to start my first course of chemotherapy on Jan 9. It was 5 straight days, about 5 hours per day, after which I would have two weeks off to recover. And then I would do it all again.
I arrived in the morning, checked in and measured my vitals (weight, blood pressure) to ensure no unexpected deviations day-to-day, and then I sat in my cozy recliner and the nurse put in an IV. It was indeed the same nurse that I met back in November.
Each day entailed dripping several full bags - first a saline solution, then side-effect (specifically nausea) mitigation medicine, and then two chemo drug bags. All of the bags took about an hour. It is a bit unsettling when the nurses don their full body protective hazmat suits while hooking up the chemo (poison) bags.
Getting chemo is mostly just boring. I would sit there on my iPad for 5 hours and then go home. I could get up and go to the bathroom, rolling along my IV pole with me. Going into it, I was wondering whether I would be able to feel the chemo drugs and whether it would sting or something. But it doesn’t. Ripping the IV tape off of my arm was the most painful part of the day. There were several dozen chemo stations in the ward, mostly full of patients all getting treatment for various forms of cancer.
On the first few days, I really didn’t feel much. I even did some light workouts. I started on a detailed regimen of 3 different oral medicines to mitigate the side effects of the chemotherapy. I had learned reading “The Emperor of Maladies,” that when Cisplatin was first administered starting in the 1970s, patients vomited on average 12 times per day. I was lucky enough to not feel any nausea throughout my entire six weeks of chemo. Thank you, Zofran!
Starting on Wednesday (2 days after starting), I did start to feel profound fatigue and, once again, had a hard time getting off of the couch. The next week, I felt terrible and really just couldn’t do much.
But by the following Saturday (8 days after ending the first cycle), I felt fine - maybe 90%. I did a hard workout and a harder one on Sunday. I finished riding the Peloton and was feeling great and put my hands over my head to wipe off all of the sweat…and noticed that my hands came back full of hair. I tugged gently on my hair, and a full tuft came out.
Here I was feeling great about having a normal hard workout, and cancer was like “nope, I’m going to make your hair fall out now.” Rather than let all of my hair fall out and make a big mess, I decided to just shave it all off then. I took my clippers outside and started shaving away, making a pile of hair in our backyard in the middle of a dark and cold New England winter afternoon. I went back inside to show my family, and they gasped as apparently I’d forgotten to use the guard on the clippers and my head was not only bald but was also streaked with blood from a bunch of cuts that I hadn’t even noticed.
I went back for my second and final full week on Jan. 30. I knew what to expect this time, but the second cycle was definitely worse. My family (both of my parents and my brother) were very generous and took turns coming to stay with us and help around the house and with the kids.
February, 2023
Recovery #3
My last day of receiving chemo treatment was Friday, February 3. I was relieved but felt like complete garbage for another 10 days or so and didn’t quite feel like celebrating yet. But towards the end of the month, I was starting to feel like myself, albeit with a lot less hair (really no hair) and I was completely and totally out of shape.

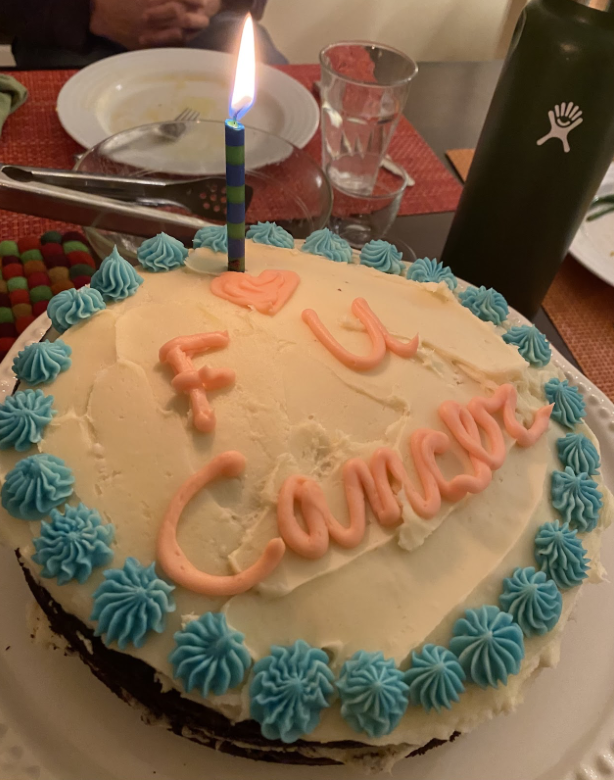
On Feb. 28th, I met with my oncologist, and he confirmed that blood work and a CT scan (my 3rd CT since August) showed no sign of cancer. I was effectively cured. In fact, he said, “To be honest, your case is a bit boring, because we are so confident in how to treat it.” I will need to do blood tests every six months and CT scans every year for the next few years, but (knock on wood) the chances of recurrence are low. That night, my family made me this cake:
Epilogue
As spring arrived, life started to return to normal. Like really normal. For the first time since August, there was no next step to take in fighting cancer. It appeared that we had won.
I was bald. But I knew it was temporary, and to be honest, I didn’t think about it very much because I don’t spend too much time looking at myself. And it was a little novel and even made me chuckle.
I am immensely thankful for the amazing medical care that I received. I think about 12 different doctors from various disciplines (Oncology, Urology, Radiology, Anesthesiology) and maybe 30 nurses and other hospital staff that were all directly and regularly involved in my care. We definitely (finally!) got our money’s worth from the insurance companies! I live in the right place (Boston) to have to go through something like this. Both surgeries and the chemo treatment were just a few miles from my house.
There are seven surgical scars on the right side of my abdomen. Four are almost impossible to see, and the other three you have to look pretty close to see, even the orchiectomy scar. That said, when I bend over to tie my shoes or the like, I can feel my insides crinkle uncomfortably. It feels a bit like my guts are forever wrapped in duct tape - remnants of the ten-hour RPLND surgery.
Since finishing treatment and trying to get back to sports, I have endured a series of basically nonstop injuries over the past two years. These are probably “regular” old man injuries, caused in no small part because I have played pounding sports for several decades. But I can’t help but wonder whether chemo and/or surgeries might have helped Father Time accelerate his inevitable victory over my body’s athletic ability.
The further I am removed from this experience, the more it starts to feel like a strange dream: “Did that really happen?” The neat and tidy narrative is that I have a new lease on life. But in reality, my perspective is more complicated. I have moments of quasi-nihilism (“Nothing matters, the cancer might come back next month, I’m going to eat another cookie”).
I also feel guilt that I was lucky enough to catch the cancer early and survive, and I think about the TC patients from 50 years ago who didn’t have access to the treatment I did and most likely would not have lived more than a few years more. I think about the other patients that were getting chemo in the ward while I was there, many of whom faced bleaker odds than I did. And I think about all of the friends and loved ones who have or will endure cancer - including several otherwise young and healthy people close to me who were diagnosed after I was and began their own battles.
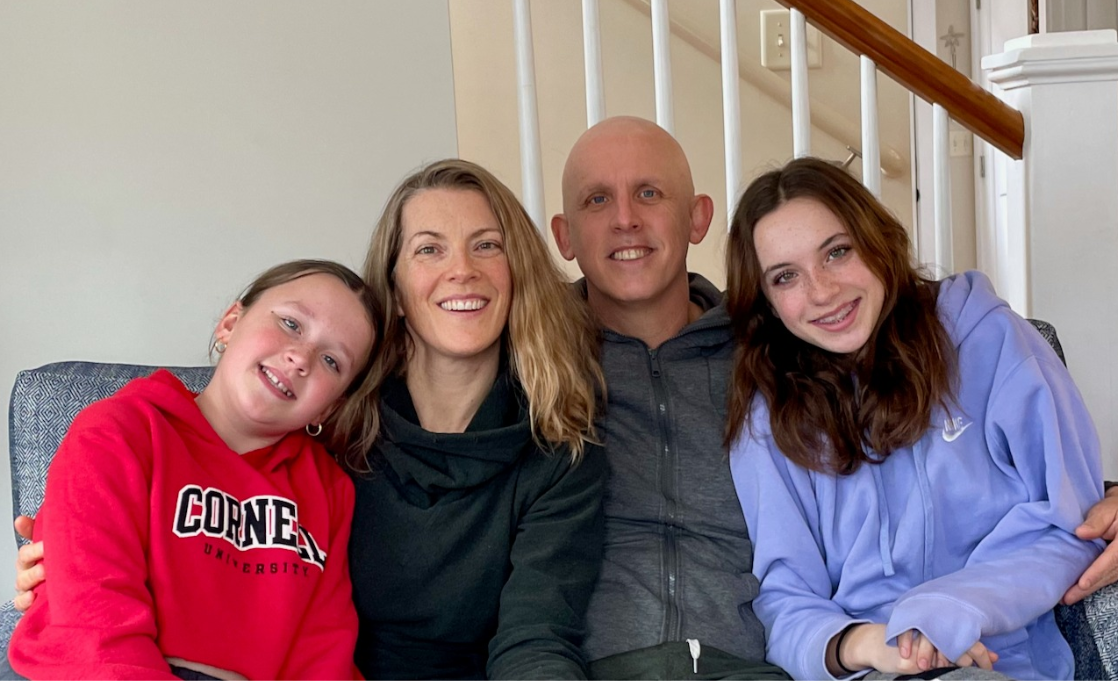
To be sure, there are also moments when I am overcome with profound gratitude for life. In July, we took a family vacation to Iceland. I was about four months removed from chemotherapy and felt fully recovered with a full head of hair (curly hair at that! I guess “chemo curls” is a thing?). We took a long hike in the beautiful and remote Thorsmork area. After a rugged and steep multiple-mile climb, we arrived at a mountain peak and were greeted by the sublime 360-degree view of a riverbed meandering between mountains draped in glistening green moss with a massive glacier as a backdrop. Taking in the sublime view, to my surprise, I was overcome with emotion and burst into tears. I started muttering “I’m still here, I’m still here…”. Anna put her hand on my back, and I turned and gave her a hug, now fully weeping. The kids giggled uncomfortably and joined in a family hug. I dried my eyes, took a deep breath, and we took the picture below.
